Cataracts
What is a cataract?
Your eye works a lot like a camera. Light rays focus through your lens onto the retina, a layer of light-sensitive cells at the back of the eye. Similar to photographic film, the retina allows the image to be “seen” by the brain.
Over time, the lens of our eye can become cloudy, preventing light rays from passing clearly through the lens. The loss of transparency may be so mild that vision is barely affected, or it can be so severe that no shapes or movements are seen—only light and dark. When the lens becomes cloudy enough to obstruct vision to any significant degree, it is called a cataract. Eyeglasses or contact lenses can usually correct slight refractive errors caused by early cataracts, but they cannot sharpen your vision if a severe cataract is present.
What causes cataracts?
The most common cause of cataract is aging. Other causes include trauma, medications such as steroids, systemic diseases such as diabetes, and prolonged exposure to ultraviolet light. People who smoke seem to get cataracts earlier than non-smokers. Occasionally, babies are born with a cataract.
Cataracts typically develop slowly and progressively, causing a gradual and painless decrease in vision. Other changes you might experience include blurry vision; glare, particularly at night; frequent changes in your eyeglass prescription; a decrease in color intensity; a yellowing of images; and in rare cases, double vision.
As the eye’s natural lens gets harder, farsighted (presbyopic) people, who have difficulty focusing up close, can experience improved near vision and become less dependent on reading glasses. However, nearsighted (myopic) people become more nearsighted, causing a worsening in their distance vision. Some kinds of cataracts affect distance vision more than reading vision. Others affect reading vision more than distance vision.
Can cataracts be prevented? Or fixed?
Reducing your exposure to ultraviolet light by wearing a wide-brimmed hat and sunglasses may reduce your risk for developing a cataract, but once one has developed, there is no cure except to have the cataract surgically removed.
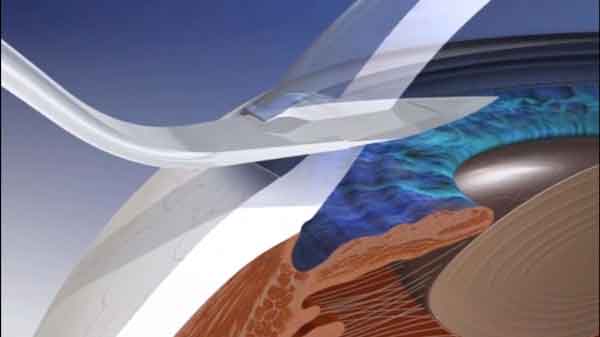
With a routine, outpatient surgical procedure, an ophthalmologist can remove the cataract by making a small incision in the cornea at the front of the eye. A synthetic intraocular lens (IOL) is inserted at the time of cataract extraction to replace the focusing power of the natural lens. IOLs can be monovision (fixed-focus for a preset distance) or multifocal, which allows focused vision at many distances. The time to have cataract surgery is when the cataract is affecting your vision enough to interfere with your normal lifestyle.

Cataract surgery is a very successful operation. One and a half million people have this procedure every year in North America, and 95% have a successful result. As with any surgical procedure, complications can occur during or after surgery, and some are severe enough to limit vision. In the vast majority of cases, vision and quality of life are improved.
Cataract Surgery: Manual or Laser?
A cloudy lens interferes with light passing through to the retina, the light-sensing layer of cells at the back of the eye. Having a cataract can be compared to looking at the world through a foggy window. Phacoemulsification is a surgical method used to remove a cataract, which is a clouding of the eye’s naturally clear lens.
In phacoemulsification, an ultrasonic oscillating probe is inserted into the eye through a small incision. The probe breaks up the center of the cataractous lens. The fragments of the cataract are then suctioned from the eye. The small incision used does not require sutures to close, since the cataract is removed in tiny pieces. The back-portion of the supportive lens capsule or “bag” is left behind and a foldable intraocular lens (IOL) is implanted permanently inside the “bag” to help focus light onto the retina. Vision returns quickly and one can resume normal tasks, within a week for most activities.
Manual Incision

Manual Capsulorhexis

Manual Phacoemulsification

Laser Incision

Laser Capsulorhexis

Laser Phacoemulsification

Replaced lens with sharp retinal focus
Learn More About Laser-Assisted Cataract Surgery
Cataract Surgery Lens Choices
Aspheric Lenses
Astigmatism Lenses
Multifocal Lenses
Multifocal IOLs, or advanced technology IOLs, are a newer type of lens that treat multiple focal points and reduces or eliminates the need for eyeglasses or contact lenses after cataract surgery. Part of the rapid evolution in IOL innovations, these newer lenses are made from cutting-edge materials with unique features. This is made possible through highly specialized optics that divide light and focus it on more than one point to provide a range from near to far eyesight Accommodative IOLs are considered monofocal, meaning they have a fixed focal point. This type of lens is designed to move in response to your eye’s own muscle, which translates into the ability to see multiple focal points.
Measurement Choices
More specifically, Atlas Zernicke Wavefront Analysis is used to identify Corneal Spherical Aberration, and this is combined with Biometry Laser Measurement which is 10 times more accurate than the basic A-scan Ultrasound measurement covered by OHIP.
Astigmatism Multifocal Lens
Laser-Assisted Cataract Surgery
The more challenging and delicate steps of cataract surgery are accomplished using a blade-free laser instead of manually performing these steps with an instrument. AEI is among the very first eye centres in Canada to offer patients this advanced technology for cataract surgery. The system provides more control to make cataract surgery more precise and allows a surgery tailored specific to patients’ eyes.
It uses image-guided, laser technology to perform the initial steps of the cataract surgery procedure with accurate and reproducible precision compared to traditional refractive cataract surgery.
Lens Replacement Packages
Titanium
For patients with or without astigmatism, this astigmatism-correcting multifocal lens implant has 3 points of focus. This package reduces pre-existing astigmatism and provides the best opportunity for glasses-free vision at all distances. Glasses may still be required (depending on your degree of astigmatism).
Gold
For patients with astigmatism, this astigmatism correcting lens implant package provides an excellent opportunity to reduce dependence on glasses for distance vision. Glasses may still be required.
Silver 
The silver package uses special measurement techniques to identify which particular aspheric lens is best suited for your unique eye. This lens provides better colour and low-light vision than the OHIP lens. Glasses may be required for reading, as well as for distance (depending on your degree of astigmatism).
OHIP
OHIP coverage includes a basic lens selected for your eye using measurements acquired with A-scan Ultrasound, a 30-year old technology. Glasses may be required for reading, as well as for distance (depending on your degree of astigmatism).
Diagnostics
Atlas Topography
 To care for your cataract, Atlas corneal topography and corneal wave front analysis are used to help plan your surgery and choose an implant that will result in the clearest vision. The Atlas Topography Unit helps determine the exact location of your astigmatism and of your cornea – both extremely important factors in determining the best way to treat your cataract. The information obtained from topography also helps improve the accuracy the calculations used to determine the power of the intraocular lens that is inserted into your eye at the time of cataract surgery. The Atlas examination is not covered by OHIP for the assessment of cataract patients. The cost of the test can be claimed on your income tax return, (Line 330 ). Atlas topography is an optional test to you, the patient. It is your choice to have an Atlas exam. It is valuable for all cataract patients and is recommended, but should you decide to decline this test the standard of care will continue to be delivered to you and every effort will be made to manage your eye condition in the best manner possible. We believe all cataract patients will benefit from Atlas topography, as it enables us to plan your cataract surgery with higher degree of precision and recommend an implant that will give you the clearest vision.
To care for your cataract, Atlas corneal topography and corneal wave front analysis are used to help plan your surgery and choose an implant that will result in the clearest vision. The Atlas Topography Unit helps determine the exact location of your astigmatism and of your cornea – both extremely important factors in determining the best way to treat your cataract. The information obtained from topography also helps improve the accuracy the calculations used to determine the power of the intraocular lens that is inserted into your eye at the time of cataract surgery. The Atlas examination is not covered by OHIP for the assessment of cataract patients. The cost of the test can be claimed on your income tax return, (Line 330 ). Atlas topography is an optional test to you, the patient. It is your choice to have an Atlas exam. It is valuable for all cataract patients and is recommended, but should you decide to decline this test the standard of care will continue to be delivered to you and every effort will be made to manage your eye condition in the best manner possible. We believe all cataract patients will benefit from Atlas topography, as it enables us to plan your cataract surgery with higher degree of precision and recommend an implant that will give you the clearest vision.Wavefront Analysis
Wavefront analysis uses a special device to precisely measure the unique irregularities and variations in the cornea. This analysis has been compared to taking a fingerprint of the eye.
With your chin resting on the device, you will be asked to stare past what is called a target light. A sensor will measure the irregularities in the wavefront pattern of the light reflecting from your cornea.
Wavefront measuring devices create a precise map of the cornea. It is very detailed and records subtle distortions in your cornea. Using the information from this map, Dr. Anjema can select the intraocular lens used in your surgery to correct for some of these measured distortions, giving you clearer vision than would be possible with conventional lenses.
Wavefront analysis is not covered by OHIP. The cost of this test can be claimed on your income tax return, (Line 330) and is optional to you, the patient.